What Causes Microscopic Colitis And Who Is Affected
As with ulcerative colitis and Crohns disease, the exact cause of microscopic colitis has yet to be identified. But bacteria, bacterial toxins, and viruses are leading candidates in research.
Some experts have suggested that use of nonsteroidal anti-inflammatory drugs , such as aspirin or ibuprofen, might be the actual culprits. It is also possible that these medications might simply aggravate symptoms in individuals who are already prone to the illness. Another theory is that collagenous colitis and lymphocytic colitis are caused by an autoimmune response, which means that the body launches an attack upon itself mistaking various cells in the colon for foreign invaders. The final answer may well turn out to be some combination of these theories.
There does seem to be a link between microscopic colitis and the autoimmune disease celiac sprue, also known as celiac disease. Caused by an immunologic reaction of the intestine to wheat, barley, rye, and oats, celiac sprue is a digestive disease that damages the small intestine and interferes with absorption of nutrients. Its hallmarks are chronic diarrhea and weight loss.
Recommended Reading: How To Cure Gastritis And Ulcers Naturally
Are Hemorrhoids A Sign Of Ulcerative Colitis
Hemorrhoids are not a classic sign of ulcerative colitis, but they can occur on top of it. In fact, people with ulcerative colitis have a higher risk of developing hemorrhoids than the general population. Thats because ulcerative colitis leads to prolonged diarrhea, which is a risk factor for hemorrhoids.
Ulcerative proctitis is a milder form of ulcerative colitis and only affects the rectum. People with ulcerative proctitis may experience:
- Bloody diarrhea
- A sense of urgency to pass stool
- A sensation of incomplete emptying after having a bowel movement
Is It More Common In Crohn’s Or Ulcerative Colitis
Rectal bleeding is more common in ulcerative colitis. Bleeding in the lower digestive tract causes bright red blood to appear. This is a more common symptom of Crohns disease, which typically affects the end of the small intestine and colon, and ulcerative colitis, the other main form of IBD which affects the colon.4
Among people with IBD, rectal bleeding is more typical of ulcerative colitis than Crohns disease.1 Bleeding related to inflammation in the colon often occurs along with diarrhea.5 and fistulas can cause bright red blood in the stool.2,4
Severe rectal bleeding can cause low blood pressure, increased heart rate, and shock.4 Hemorrhage leads to hospitalization in 1.2% of patients with Crohns disease and 0.1% of ulcerative colitis.4
You May Like: Where Do I Go For Hemorrhoids
Symptoms Of Ulcerative Proctitis
The presenting symptoms of ulcerative proctitis all relate to the rectum. Blood in the stool occurs in almost everyone with the disease. Diarrhea is a common symptom, although constipation can also develop as the body struggles to maintain normal bowel function.
Inflammation of the rectum may cause a sense of urgency to have a bowel movement, discomfort after having a bowel movement, and a sensation of incomplete emptying of the bowels. Systemic symptoms such as fever, tiredness, nausea, and weight loss are rare.
Who Diagnoses Ulcerative Colitis

If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Recommended Reading: Is Ice Cream Good For Hemorrhoids
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Treatment Of Ibd Complications
Treatment depends on the particular complication, but may include:
- complications caused by nutritional deficiencies vitamin and mineral supplements , changes to diet or a liquid diet in severe cases
- inflammation in other body areas usually ease when the bowel inflammation is controlled with medication
- fistulas small openings that often heal by themselves, with treatment to ease the inflammation. A person may need surgery to close a larger fistula. Abscesses may need antibiotics and surgical drainage
- intestinal obstruction in some cases, medical treatment to ease the inflammation will clear the obstruction. In severe cases, the person will need surgery
- toxic megacolon the person goes to hospital, and receives fluids and nutrients intravenously instead of by mouth, plus antibiotics and steroids to reduce inflammation. Sometimes, the doctor will remove the contents of the persons stomach with a slender tube . A ruptured bowel needs surgical repair or removal. In severe cases, the whole of the large bowel may need to be surgically removed.
You May Like: Can Internal Hemorrhoids Cause Pain
The Difference Between Sigmoidoscopy And Colonoscopy
Both sigmoidoscopy and colonoscopy use a camera attached to a thin flexible tube to help doctors view the inside of the large intestine. There are some major differences between the two, though. The primary differences are the areas of the intestines examined and the conditions each can detect.
Colonoscopy is a thorough examination of the large intestine in its entirety, from the cecum to the sigmoid colon.
Doctors use colonoscopies to diagnose a number of digestive conditions, including:
In a sigmoidoscopy, doctors examine only the rectum and the sigmoid. A sigmoidoscopy helps doctors diagnose ulcerative colitis and polyps that might become colon cancer.
A sigmoidoscopy is less invasive than a colonoscopy, so doctors often start with a sigmoidoscopy if they suspect a condition affecting only the sigmoid and not the rest of the colon. Doctors typically recommend that patients undergo colonoscopy if they find polyps on sigmoidoscopy, as if polyps develop in the sigmoid colon, they are likely to develop elsewhere.
For more information on colonoscopies and sigmoidoscopies, or to learn more about each of these important procedures, contact the GI professionals at Allied Digestive. Our gastroenterologists are glad to help.
What Causes Rectal Bleeding
In general, hemorrhoids and diverticular disease are the most common causes of rectal bleeding.2,5 Other common causes include:
- Angiodysplasia of the colon
- Colon inflammation from many causes
- Stomach ulcers
- Colorectal cancer
Bleeding in the lower digestive tract has been linked to taking non-steroidal anti-inflammatory drugs , such as Aleve, Advil, and Motrin.4 Once you have been diagnosed with IBD, NSAIDs are not recommended.6
However, research about the link between NSAIDs and IBD is ongoing and so far, inconclusive. No studies have shown that taking these medications is a cause of IBD.7
Also Check: What Type Of Doctor Do You See For Hemorrhoids
What Are The Treatments For Hemorrhoids
If at-home treatments for hemorrhoids don’t help you, you may need a medical procedure. There are several different procedures that your provider can do in the office. These procedures use different techniques to cause scar tissue to form in the hemorrhoids. This cuts off the blood supply, which usually shrinks the hemorrhoids. In severe cases, you may need surgery.
Ulcerative Colitis Risk Factors
Most people with UC dont have a family history of the condition. However, about 12 percent of people with UC do have a family member with IBD, according to research from 2014.
UC can develop in a person of any race, but its more common in white people. If youre of Ashkenazi Jewish descent, you have a greater chance of developing the condition than most other groups.
Young people with IBD may also be dealing with acne at the same time. Some older studies have suggested a possible link between the use of the cystic acne medication isotretinoin and UC. However, newer research has yet to find a definitive causal relationship.
Theres no solid evidence indicating that your diet affects whether you develop UC. You may find that certain foods and drinks aggravate your symptoms when you have a flare-up, though.
Practices that may help include:
- drinking small amounts of water throughout the day
- eating smaller meals throughout the day
- limiting your intake of high fiber foods
- avoiding fatty foods
- lowering your intake of milk if youre lactose intolerant
Also, ask a doctor if you should take a multivitamin.
Recommended Reading: Does Colon Cancer Cause Hemorrhoids
Is Ulcerative Colitis Curable
Currently, theres no nonsurgical cure for UC. Treatments for the inflammatory disease aim to extend periods of remission and make flare-ups less severe.
For people with severe UC, curative surgery is a treatment option. Removing the entire large intestine will end the symptoms of UC.
This procedure requires your doctor to create a pouch on the outside of your body where waste can empty. This pouch can become inflamed and cause side effects.
For that reason, some people choose to have only a partial colectomy. In this surgery, your doctor only removes the parts of the colon that are affected by UC.
While these surgeries can help ease or end symptoms of UC, they can have adverse effects and possible long-term complications. Read more about these issues to determine if surgery is an option for you.
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Recommended Reading: Why Do My Hemorrhoids Bleed So Much
Colectomy Proctocolectomy And Ileostomy
If Crohn disease becomes extremely severe, and other treatments do not help, the entire colon may need to be removed. If the rectum is also affected, it will also need to be removed:
- Colectomy is surgical removal of the entire colon
- Proctocolectomy is surgical removal of the entire colon and rectum
People who have a colectomy still retain their rectums and are able to pass stool naturally. Because proctocolectomy involves removing the rectum, the surgeon must perform another procedure, called ileostomy, after proctocolectomy to create an opening to allow waste to pass through.
Proctocolectomy with ileostomy involves the following:
- To perform proctocolectomy, the surgeon removes the entire colon, including the lower part of the rectum and the sphincter muscles that control bowel movements.
- To perform ileostomy, the surgeon makes a small opening in the lower right corner of the abdomen called a stoma. The surgeon then connects cut ends of the small intestine to this opening. An ostomy bag is placed over the opening and accumulates waste matter. It requires emptying several times a day.
What Makes This Hemorrhoids Breakthrough So Exciting Is That It Gives You The Power Todifference Between Hemorrhoid And Colitis
Difference Between Hemorrhoid and Colitis Hemorrhoid No MoreT is a 150 page downloadable e-book, jam-packed cover to cover with all the secret natural Hemorrhoids cure methods, unique powerful techniques and the step-by step holistic Hemorrhoids system Ive discovered in over 14 years of research. This program contains all the information youll ever need to eliminate your Hemorrhoids permanently in weeks, without using drugs, without surgery and without any side effects.
Recommended Reading: How To Treat Small Hemorrhoids
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
What Supplements Should You Take For Crohns Disease Vs Ulcerative Colitis
Crohns disease nutritional diet deficiencies
- Your need for vitamin and mineral supplements depends on several factors, your diet, which parts of your digestive tract are affected, and whether you have had surgery on your small intestine.
- The most common vitamin deficiencies are
- vitamins D and B-12.
Ulcerative colitis nutritional deficiencies
As with Crohns disease, nutrition is important if you have ulcerative colitis because symptoms of diarrhea and bleeding can lead to dehydration, electrolyte imbalance, and loss of nutrients. It may be necessary to take nutritional supplements if your symptoms do not allow you to eat a nutritionally balanced diet. Talk to your health-care professional about what supplements to take.
Don’t Miss: Can You Use Hydrocortisone Cream On Hemorrhoids
You And Your Care Team Are In Control
While there is no cure for UCwhile also knowing it can progress and symptoms can get worse over timeits important to remember that you and your doctor can get your disease under control. Recognizing the signs early and getting treatment right away is key. Thats why having open conversations with your doctor and being prepared for every appointment is crucial to managing your UC.
Speak openly with your doctor about how much your UC is truly impacting you. Make a personal action plan to see how much of your time your disease is affecting and get customized steps to help you and your doctor get control of your disease.
You May Like: What Foods Not To Eat If You Have An Ulcer
Uc Results In Chronic Or Long
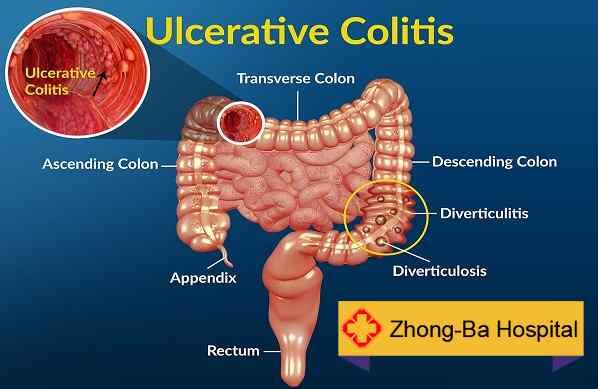
Ulcerative colitis is one of the two common types of inflammatory bowel disease that affects the large intestine, also known as the colon. The other one is Crohn’s disease.
The condition eventually contributes to the development of ulcers in the lining of the colon. It’s not curable, but there are ways to manage symptoms.
Also Check: How To Get Rid Of Hemorrhoids Postpartum
Hemorrhoids Are A Very Common Ailment In Both Men And Women
Hemorrhoids are a very common ailment in both men and women. About 75% of all people will have hemorrhoids at some point in their lives, and about half will have them after the age of 50. Thats little solace to someone suffering from any painful symptoms, but worth knowing nonetheless. There should be no shame or taboo associated with the condition.
A quick primer before we look at understanding the symptoms that hemorrhoids present as compared to other ailments with similar symptoms:
There are lots of different causes of hemorrhoids, the most common of which are:
- Chronic Constipation or Diarrhea
- Eating a low-fiber diet
- Regular heavy lifting
Now that we understand the fundamentals of the disease, we can delve deeper into differentiating hemorrhoids from other conditions with similar symptoms.
References: