Risk Factors For Hemorrhoids
Several risk factors have been claimed to be the etiologies of hemorrhoid development including aging, obesity, abdominal obesity, depressive mood and pregnancy. Meanwhile, some conditions related to increased intraabdominal pressure, such as constipation and prolonged straining, are widely believed to cause hemorrhoids as a result of compromised venous drainage of hemorrhoid plexus. Some types of food and lifestyle, including low fiber diet, spicy foods and alcohol intake, was reported to link with the development of hemorrhoids and the aggravation of acute hemorrhoid symptoms.
How Do Doctors Treat Hemorrhoids
Doctors treat hemorrhoids with procedures during an office visit or in an outpatient center or a hospital.
Office treatments include the following:
- Rubber band ligation. Rubber band ligation is a procedure that doctors use to treat bleeding or prolapsing internal hemorrhoids. A doctor places a special rubber band around the base of the hemorrhoid. The band cuts off the blood supply. The banded part of the hemorrhoid shrivels and falls off, most often within a week. Scar tissue forms in the remaining part of the hemorrhoid, often shrinking the hemorrhoid. Only a doctor should perform this procedureyou should never try this treatment yourself.
- Sclerotherapy. A doctor injects a solution into an internal hemorrhoid, which causes scar tissue to form. The scar tissue cuts off the blood supply, often shrinking the hemorrhoid.
- Infrared photocoagulation. A doctor uses a tool that directs infrared light at an internal hemorrhoid. Heat created by the infrared light causes scar tissue to form, which cuts off the blood supply, often shrinking the hemorrhoid.
- Electrocoagulation. A doctor uses a tool that sends an electric current into an internal hemorrhoid. The electric current causes scar tissue to form, which cuts off the blood supply, often shrinking the hemorrhoid.
Outpatient center or hospital treatments include the following:
Sometimes complications of hemorrhoids also require treatment.
Future Perspectives In The Treatment Of Hemorrhoids
To date, it is obvious that, apart from oral flavonoids-based phlebotonic drugs, currently available medication for hemorrhoids has no or limited beneficial effects on bleeding and prolapsing. Since emerging evidence has suggested that perivascular inflammation, dysregulation of the vascular tone and vascular hyperplasia could play an important role in the development of hemorrhoids, the microcirculatory system of hemorrhoid tissue could be a potential and robust target for medical treatment. The combinations of vasoconstrictive and venoconstrictive agents, with or without anti-inflammatory drugs, might be a new pharmacological approach for hemorrhoids.
If an intervention, either office-based procedure or surgery – is indicated, evidence-based approaches must be exercised. Day-case operation or ambulatory surgery should be fully developed together with an effective program for peri-operative care. Despite advances in office-based procedures and better surgical approaches, post-procedural pain and disease recurrence remain the most challenging problems in the treatment of hemorrhoids. Consequently, future researches and novel management of hemorrhoids may focus on how to minimize pain following a procedure and how to prevent recurrent hemorrhoids. Meanwhile, long-term results of newly or recently developed interventions are definitely required.
Also Check: Who To Go To For Hemorrhoids
Acutely Thrombosed Or Strangulated Internal Hemorrhoids
Patients with acutely thrombosed or strangulated internal hemorrhoids usually present with severely painful and irreducible hemorrhoids. The incarcerated hemorrhoids may become necrotic and drain. This situation is quite difficult to treat particularly in a case of extensive strangulation or thrombosis ,3A), or the presence of underlying circumferential prolapse of high-graded hemorrhoids. Manual reduction of the hemorrhoid masses, with or without intravenous analgesia or sedation, might help reducing pain and tissue congestion. Urgent hemorrhoidectomy is usually required in these circumstances. Unless the tissues are necrotic, mucosa and anoderm should be preserved as much as possible to prevent postoperative anal stricture. In expert hands, surgical outcomes of urgent hemorrhoidectomy were comparable to those of elective hemorrhoidectomy.
Complicated hemorrhoids. A: Strangulated internal hemorrhoid B: Acutely thrombosed external hemorrhoid.
Just Walk In For Hemorrhoid Treatment
Hemorrhoid treatment varies from multiple measures you can do at home to minimally invasive medical procedures. Treatment options depend on the severity, frequency, and type of hemorrhoids you have and any related issues you may be experiencing. Our health care providers can offer you a plan that involves both pain relief and prevention of future hemorrhoids.
In some extreme cases, surgical removal becomes necessary either when a person has large protruding hemorrhoids or their hemorrhoids do not respond to other treatments. However, youll need a professional medical exam to determine if this is the case. Dont diagnose yourself, and dont live with the pain! Get hemorrhoid treatment today.
MEDIQ Urgent Care understands that some people feel more comfortable making an appointment for hemorrhoid treatment. If youre one of those people, you can always call our office to schedule a visit, or you can use our online tool to register for an appointment time. Either way, youll still receive the same great care!
Want to make your check-in move more quickly the day of your visit? Download this patient registration form and bring a completed copy with you when you come in.
Don’t Miss: What Is The Best Home Treatment For Hemorrhoids
How Are Hemorrhoids Treated
For most external hemorrhoids, home treatment is all you need. This includes slowly adding fiber to your meals, drinking more water, and using an ointment to stop itching. The same treatment can be used for most internal hemorrhoids. If your hemorrhoids are severe, you may need medical treatment to shrink or remove them.
Advantages Of The Procedure
- No hospitalizations
- No general anesthesia
- Less time lost from work most patients return to work and resume normal activities the same day
- Fewer serious complications in this procedure
- With this method, the early recurrence rate is reduced to about 15% and late recurrences average about 20%. Hemorrhoids may recur if you strain during bowel movements, sit on the toilet and read, etc.
Recommended Reading: How To Help Poop With Hemorrhoids
Understanding And Examining Hemorrhoids
What Is Meningococcal Disease
Meningococcal disease is any illness or condition caused by the Neisseria meningitidis bacteria, which are often severe illnesses that can result in death. The bacteria are transmitted through respiratory secretions, meaning spit and saliva. However, it takes close contact for transmission to occur .Meningococcal disease most often affects the spinal cord and brain lining, but may also cause infections within the bloodstream. Protect yourself and your children from this disease by scheduling a meningococcal vaccine today.
You May Like: What Can Help Hemorrhoids Go Away
What Are The Signs And Symptoms Of An Internal Or Prolapsed Hemorrhoid
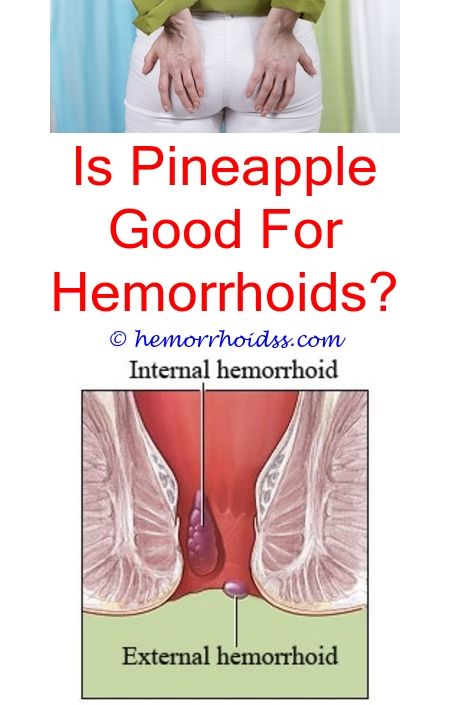
Most often, internal hemorrhoids have no symptoms but are only found if there is bleeding with a bowel movement or if the hemorrhoid prolapses so that it can be felt outside of the anus. This may lead to itching and pain as well as the bleeding.
Prolapse of an internal hemorrhoid occurs when the internal hemorrhoids swell and extend from their location in the rectum through the anus. A prolapsed internal hemorrhoid:
- Can be felt as a lump outside the anus
- Can be gently pushed back through the anus, this may resolve the location of the hemorrhoid, but does not fix the hemorrhoid itself
- May enlarge and swell even more if it cannot be pushed back
- May become entrapped, which requires more urgent medical attention
Hemorrhoids may also cause anal itching , and a constant feeling of needing to have a bowel movement .
Internal hemorrhoid severity can be graded:
- Grade I: Prominent blood vessels with no prolapse
- Grade II: Prolapse with bearing down but with spontaneous reduction
- Grade III: Prolapse with bearing down but requiring manual reduction
- Grade IV: Prolapse with inability to manual reduction
Who To See For Hemorrhoids
In most cases, your or primary care physician can help you manage hemorrhoids. However, if the hemorrhoids are severe, you may need to see a hemorrhoid doctor, such as a or a . These providers can provide more advanced hemorrhoid treatment, such as:
-
Rubber band ligation: A surgeon places a special medical-grade rubber band round the base of the hemorrhoid to cut off blood circulation. Within a week, the end of the hemorrhoid shrivels and falls off, leaving behind scar tissue.
-
: This is an out-patient surgical procedure to remove the hemorrhoids.
-
Hemorrhoid stapling: Used primarily for internal hemorrhoids, this procedure uses a stapling tool that removes tissue.
-
Sclerotherapy: This involves an injection of a chemical solution directly into the hemorrhoid to shrink it.
-
Infrared photocoagulation: Used only for internal hemorrhoids, this procedure directs an infrared light towards the tissue to cause scars, which block blood flow to the hemorrhoids.
-
Electrocoagulation: Similar to infrared photocoagulation, this procedure uses electric current to cause scar tissue.
Some people may be embarrassed to speak with their doctor about hemorrhoids, but the condition is so common that your doctor wont be surprised if you bring it up. Theres no need to live with the pain and discomfort of hemorrhoids. Prompt treatment will allow you to live your life more comfortably.
Also Check: What Can I Do To Treat Hemorrhoids
Early Postoperative Complications Of Anorectal Surgery
Since many anorectal procedures can be performed safely and effectively in an ambulatory setting or an overnight stay, some patients may develop complications sooner or later after hospital discharge. Common early postoperative complications that bring patients back to the hospital include acute urinary retention, bleeding, fecal impaction and anorectal sepsis.
The incidence of acute urinary retention following benign anorectal surgery ranges from 0.5% to 17% depending on the extent of surgery, anesthetic technique, analgesic method, amount of intravenous fluid given and patients underlying disease. Bladder catheterization is the standard treatment of acute postoperative urinary retention. Should the volume of urine is less than 600 mL in low-risk individuals, the patients may be sent home without voiding. But if the catheterized urine volume exceeds 600 mL especially in high-risk patients , a self-retaining Foley catheterization may be required before discharge.
Acutely Thrombosed External Hemorrhoids
Acutely thrombosed external hemorrhoids often develop in patients with acute constipation, or those with a recent history of prolonged straining. A painful bluish-colored lump at the anal verge is a paramount finding .3B). The severity of pain is most intense within the first 24-48 h of onset. After that, the thrombosis will be gradually absorbed and patients will experience less pain. As a result, surgical removal of acute thrombus or excisional hemorrhoidectomy may be offered if patients experience severe pain especially within the first 48 h of onset. Otherwise, conservative measure will be exercised including pain control, warm sitz baths, and avoidance of constipation or straining. A resolving thrombosed external hemorrhoid could leave behind as a residual perianal skin tag -which may or may not require a subsequent excision.
Recommended Reading: Can You Band Your Own Hemorrhoids
Hemorrhoids In Patients Having Anticoagulant Or Antiplatelet Drugs
Anticoagulant or antiplatelet drugs may promote anorectal bleeding in patients with hemorrhoids and increase risk of bleeding after banding or surgery. Unless the bleeding is persistent or profound, the discontinuity of antithrombotic drugs may be unnecessary because most of the bleeding episodes are self-limited and stop spontaneously. Conservative measure is therefore the mainstay treatment in these patients. Injection sclerotherapy is a preferential treatment for bleeding low-graded hemorrhoids refractory to medical treatment. Rubber band ligation is not recommended in patients with the current use of anticoagulant or antiplatelet drugs due to the risk of secondary bleeding. If banding or any form of surgery for hemorrhoids is scheduled, the cessation of anticoagulant or antiplatelet drugs about 5-7 d before and after the procedure is suggested.
Iv Fluids For Dehydration
There are any number of reasons why your body may become dehydrated. Sweating, vomiting, diarrhea, or simply not drinking enough water can all result in fluid loss requiring rehydration. Common symptoms of dehydration include confusion, weak or rapid pulse, fatigue, dizziness, and nausea. If your dehydration is serious, your FastMed clinician may recommend replacement of essential fluids and electrolytes via intravenous infusion.
Don’t Miss: Who Do You See For Hemorrhoids
Contemporary Pathophysiology Of Hemorrhoids
The exact pathophysiology of hemorrhoids is poorly understood. Currently, hemorrhoids is the pathologic term describing symptomatic and abnormally downward displacement of normal anal cushions. As a result of destructive changes in the supporting connective tissue and abnormal blood circulation within anal cushions, the sliding anal cushions embrace abnormal dilation and distortion of hemorrhoid plexus. A recent study of morphology and hemodynamic of arterial supply to the anal canal revealed a hyperperfusion state of hemorrhoidal plexus in patients with hemorrhoids, suggesting the dysregulation of vascular tone within hemorrhoid tissue. Moreover, it was evident that hemorrhoidal tissue contained some inflammatory cells and newly-formed microvessels. For circumferential prolapsing hemorrhoids, these might be related to an internal rectal prolapse. In conclusion, although the true pathophysiology of hemorrhoid development is unknown, it is likely to be multifactorial – including sliding anal cushion, hyperperfusion of hemorrhoid plexus, vascular abnormality, tissue inflammation and internal rectal prolapse . The different philosophies of hemorrhoid development may lead to different approaches to the treatment of hemorrhoids.
More Than 80% Of Americans Will Develophemorrhoids At Some Point In Their Liferelief Is Here Now
SENIORS
Hemorrhoids affect approximately 80% of Americans at some time in their lives. Hemorrhoids become more common and more problematic as we age. HemWell America has helped many Seniors get back to living an active lifestyle.
ACTIVE ADULTS
Hemorrhoids are most common among adults ages 45 to 70. Many will choose to compromise their once active lifestyles in order to accommodate symptoms and avoid surgery. Wait no more. Stop suffering and get back in the game of life.
POSTPARTUM
Postpartum hemorrhoids is a common condition among women. HemWell America is committed to helping new moms eliminate the symptoms of hemorrhoids and return to normal activities as quickly as possible.
ATHLETES
As an athlete, you push your body to the limit on a regular basis and repetitive exercise over long periods of time can worsen hemorrhoids. This is a new approach to a proven procedure. It is a quick, easy, safe, and effective 5 minute in-office procedure.
Don’t Miss: How To Check For Hemorrhoids
How To Treat Hemorrhoids And When You Should See Your Doctor
Hemorrhoids are an irritating, often painful condition that occurs when the veins around the anus or lower part of the rectum become swollen and inflamed as a result of too much pressure. External hemorrhoids develop underneath the skin around the anus, while internal hemorrhoids develop in the lining of the tissues.
Hemorrhoids affect about 1 in 20 Americans, and about half of adults over age 50 have them. Age is one factor as we get older, the supporting tissues in the rectum and anus become weaker and more vulnerable to pressure.
Pregnancy also can weaken these tissues, which is why pregnant women often experience hemorrhoids. Other potential causes include chronic constipation or diarrhea, straining during bowel movements and sitting on the toilet for extended periods. Also, frequently lifting heavy objects may increase the likelihood of hemorrhoids.
What are the symptoms of hemorrhoids?
Hemorrhoid symptoms vary depending on whether the inflamed veins are external or internal.
External hemorrhoids may cause itching and pain, especially while seated. Also, you may feel one or more tender lumps around the anal area. Scratching, rubbing or excessively cleaning the area can make symptoms worse.
With internal hemorrhoids, you may notice bright red blood when you have a bowel movement. Internal hemorrhoids are not usually painful unless they fall through the anal opening, called prolapsing.
How are hemorrhoids treated at home?
When to see the doctor
Related tags:
When Should You Go To The Doctor For Hemorrhoids
Again, before assuming that your condition is hemorrhoids, it’s a good idea to see your doctor for an examination. After all, it’s difficult to take a look for yourself. If there is any bleeding, severe pain or fecal incontinence , you should definitely see the doctor. A large amount of bleeding or the sudden onset of severe pain means you should seek medical treatment immediately.
You May Like: Can You Get Laser Hair Removal With Hemorrhoids
Hemorrhoids Are Common So Dont Be Shy About Seeking Relief
Most people dont want to talk about hemorrhoids. But keeping silent could stand in the way getting relief for a condition thats very common. And your doctor certainly doesnt mind addressing the topic of hemorrhoids. In fact, they want to discuss your symptoms. Because what you think is a hemorrhoid could be something more serious. Its best to get your hemorrhoids checked out early, for your peace of mind and to protect your health.Doctors have seen and heard everything, so you dont have to feel embarrassed when talking about hemorrhoids especially since nearly half of all adults experience them by age 50, says Dr. Christopher Buzas, a colorectal surgeon at Geisinger. However, its essential to get a medical diagnosis to rule out other conditions, like colon cancer or irritable bowel syndrome, and not rely on your own opinion about whats causing the problem.